When you turn 65, the federal government will start picking up the cost of most of your medical needs, and you’ll be paying far less in health care premiums. But the transition from private insurance to the Medicare program isn’t quite as easy as you might have hoped. You’ll have to make decisions that could affect which doctors and hospitals you’ll be able to see and how much you’ll have to pay out of pocket for your health care.
Let’s start with the easy part. If you are already receiving Social Security benefits, you’ll get your red, white and blue Medicare card in the mail around three months before your 65th birthday. You’ll be enrolled in Part A, which pays for hospital coverage and costs you nothing as long as you or your spouse paid Medicare taxes for at least 40 quarters, the equivalent of 10 years.
Part B, on the other hand, which picks up a large part of the tab for doctors’ bills and other medically necessary services, costs $134 per month for most people who enrolled for the first time in 2018. If you are already getting Social Security, that amount will be deducted from your check. If you aren’t, you’ll have to pay for Part B separately, either monthly or quarterly, through a bank draft, with a credit card or by mailing a check or money order to the Medicare Premium Collection Center in St. Louis.
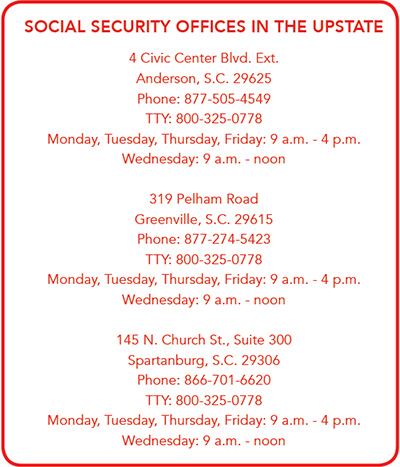
If you aren’t receiving Social Security benefits, you’ll have to apply for Part A and Part B, either online at www.ssa.gov, by calling 800-772-1213 or by visiting the local Social Security office in Greenville, Spartanburg or Anderson.
Kim Reyes, a benefits counselor with the Appalachian Area Agency on Aging, pointed out that you have a seven-month window to apply for Part A and Part B. Your initial enrollment period includes the month you turn 65 and the three months before and after. If you don’t have health insurance, either from your employer or your spouse’s employer, for example, and you wait to sign up for Part B, you’ll have to pay a 10-percent penalty for every year you could have enrolled but didn’t.
That’s the easy part. The more complicated aspect of signing up for Medicare is choosing who, if anyone, will foot the bill for the deductibles, co-pays and other items not covered by Medicare. For example, Reyes noted that there is a $1,340 deductible for hospital stays, a number that is subject to change from year to year. In addition, you would be responsible for $329 a day for days 61 through 90 and $658 a day after 91 days in the hospital. You also must pay a $183 annual deductible under Part B, along with 20 percent of your doctors’ bills and other outpatient services, such as therapies, outpatient surgery, diagnostic testing and durable medical equipment.
You can buy insurance from a private company to cover these expenses. With a Medigap plan, you can choose from among 10 separate options, A, B, C, D, F, G, K, L, M or N, each offering different services, co-payments and deductibles. Reyes pointed out that plans F and C will no longer be sold after 2020, though Medicare recipients who already have those plans will be able to keep them.
The coverage provided under these Medigap plans offers identical benefits from carrier to carrier; the difference is what each private company charges, according to Hal Zoller, president of Resource Equity Group of Greenville.
“It’s a matter of shopping around and getting the best price,” said Zoller. “The benefits are dictated by the federal government. You should talk to a qualified agent, not the carrier. You might talk to two or three independent agents that have no bias and get their input.”
Your other option is a Medicare Advantage plan, also offered by private companies. Reyes said these plans provide all your hospital and medical coverage and sometimes additional coverage for vision, dental, hearing, gym membership and prescription drugs.
“The downside is that you might be limited to certain doctors and hospitals,” Reyes said.
According to Zoller, one of the biggest changes in the Medicare landscape from 2018 to 2019 is that several carriers are now offering “extremely rich” Medicare Advantage options. Some even have no premiums and a “give back” benefit that subsidizes part of your Part B premium every month.
Medicare Advantage plans come in two basic forms. In a health maintenance organization, or HMO, you are limited to doctors, hospitals and other providers in your local service area, with no coverage outside that network. With a preferred provider organization, or PPO, you may use any provider in the company’s network, and you are covered at a lower level if you use a provider that isn’t in the network. Many PPOs have providers nationwide, which gives you some flexibility to seek treatment anywhere in the United States.
Reyes noted that in 2019, those enrolled in Medicare Advantage plans will have an additional enrollment period that lasts from Jan. 1 through March 31. During that time, beneficiaries may move to a different Advantage plan or choose to return to original Medicare and opt for a Part D plan to pay for prescription drugs.
If you don’t have a Medicare Advantage plan that pays for prescriptions, you’ll need to enroll in a Medicare Advantage Prescription Drug Plan. Neither original Medicare nor Medigap plans cover drugs.
“You want to get the most bang for your buck, based on your budget,” Reyes concluded. “It’s not one size fits all. I always tell people you don’t buy homeowners insurance because you don’t want your house to burn down. People need to do their homework and know exactly what their coverage is.”
By Brian Sherman
