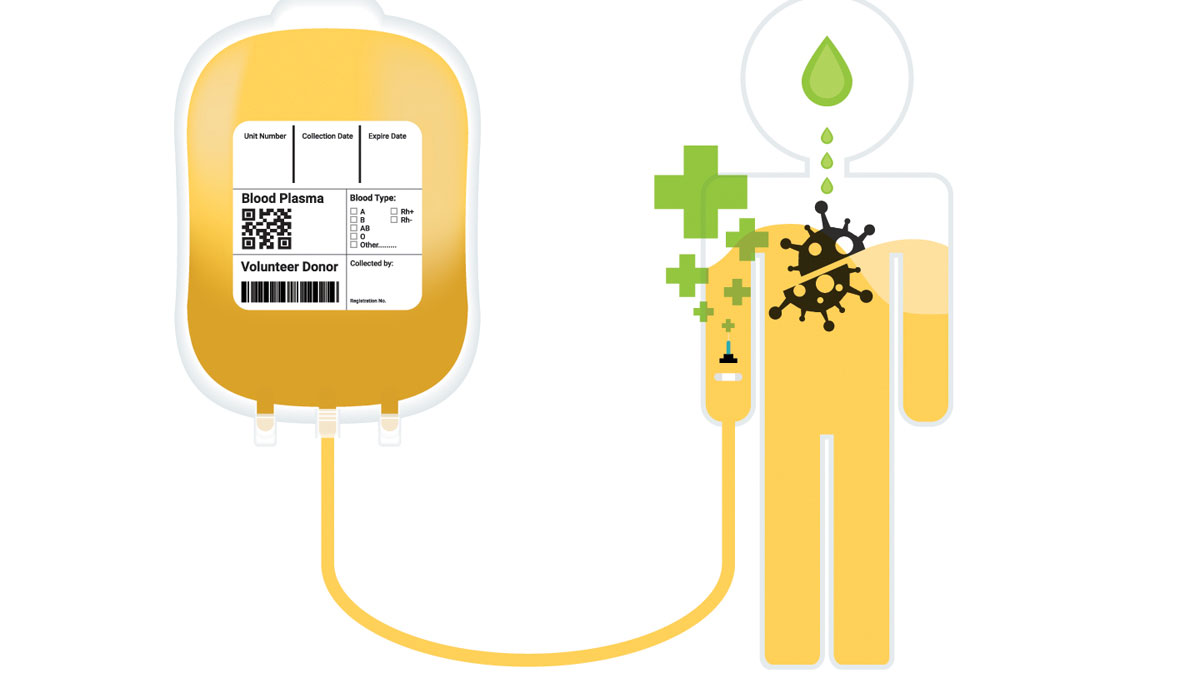
Convalescent plasma therapy is not a new medical treatment. However its significance has grown recently as a valuable tool for patients currently fighting the coronavirus. Plasma therapy has a variety of purposes and is regularly utilized to help patients fight infection through the transfer of antibodies from the donor to the patient. Plasma therapy is authorized by the FDA to help COVID-19 patients recover faster and, on the front lines, medical care teams and blood centers are working together to meet its extraordinary demand.
John McEvoy, M.D., director of molecular pathology services at Coastal Pathology Laboratories and director of pathology at Roper St. Francis Healthcare in Charleston, explained that there is an extensive history of using convalescent plasma therapy for infections.
“We’ve used plasma from one patient to another to help treat infections for about 100 years. That comes from this idea: I had an infection, whether it was flu or COVID, and I made antibodies to fight that infection. Then you had COVID or the flu. We could take my plasma, provided that it matched your blood type, and give you that plasma,” said Dr. McEvoy.
The overall efficacy of plasma therapy against COVID-19 is hard to determine, but positive results have been shown in specific patients, said Dr. McEvoy.
“It has shown benefit in COVID patients. I would say mild to modest benefit. It seems to have the most benefit if it is given to the patients in the first couple of days,” he added.
Many factors must be considered before a specific patient receives the treatment. Plasma is a finite, patient-provided resource, and that alone makes administering the treatment an important decision for providers. At the same time, it seems like it is most useful if given early on, so the care team’s decisions must be swift.
“We weigh it between, ‘Do we think that early on this patient could be somebody that would benefit from it, and maybe spare them a severe course of COVID?’ ‘Then if we wait too long because they seem to be having a mild course, have we missed the best window for administration?’” shared Dr. McEvoy.
While plasma therapy appears to benefit COVID-19 patients, it is not a cure like some had hoped for early on in the pandemic. Instead, doctors say it’s an important tool in an array of treatments that are being used to combat the effects of the virus.
“It’s not been the great panacea that the media made it out to be in March or April, but, frankly, nothing has been. I think that it is one of a number of things that we’ve utilized over the last eight or nine months to help patients recover faster,” said Dr. McEvoy.
Fortunately, hospitals and care teams aren’t alone in the process. Blood centers are responsible for collecting it from donors and distributing it to the hospitals, where it is administered. The Blood Connection, which serves the Carolinas, partners with Roper Hospital to provide plasma and other blood products. Allie Van Dyke, partnerships and media coordinator, shares the importance of COVID-19 plasma donations in The Blood Connection’s public outreach.
In addition to regular blood donations, blood centers that collect plasma specifically for COVID-19 patients face a specific set of criteria for donors. For instance, only former COVID-19 patients with antibodies are able to donate plasma for current COVID-19 patients, and they must be completely recovered, healthy and feel well enough to donate. These requirements and others severely limit the number of people who are able to donate and, as a result, the amount of donor plasma available for patients who are ill.
“When you take all of that into consideration, it’s a small group of people we’re talking to here with this huge need in the community, but we only have a small percentage of the community who can actually do this,” said Van Dyke
Once a potential donor feels well enough to donate, the process is rather simple and straightforward.
“It’s very similar to an actual blood donation – it’s just longer. It’s still a single needle stick, but what we do is connect the donor to a large machine that is filtering out the plasma and giving the donor the rest of the blood back through the same needle,” said Van Dyke. “You’re in your chair for a regular blood donation for a maximum of 15 minutes, but you can be in the donation bed for about an hour to an hour-and-a-half with a plasma donation, so that’s really the main difference is the length of time.”
For the donor, everything from the screening process and sticking process to the refreshment is the same. Since only the plasma is removed from the donor and not platelets or red blood cells, some donors say the recovery time is a little faster than with a regular blood donation.
“People actually say they feel a little better after an apheresis donation, which is plasma or platelets or anything other than whole blood,” said Van Dyke. “Because you are getting some of the blood back, your body recovers a little quicker, and people say they feel a little better.”
Antibody screening and plasma donation is free for donors at The Blood Connection – which encourages all potential donors to be screened, especially those who have tested positive and recovered from COVID-19 and those who suspect they may have had COVID-19 or may have been asymptomatic. It’s recommended that donors make an appointment ahead of time by calling 864-751-1168. There are donation centers located throughout the Carolinas.
By Katie Thompson