Detoxification is an important component of a patient’s recovery process from opioid use disorder. Medical experts share that while the detox process is difficult and uncomfortable, it shouldn’t be a deterrent in keeping someone with a substance use disorder from getting help.
“When I was in the grips of my opioid addiction, the only thing that had a stronger hold on me was fear. Fear of being judged by society, by my friends and even by my family. Fear of the physical, mental and emotional pain of withdrawal. That fear kept me sick for a long time,” said Dominic Rosa, director of business development at Lantana Recovery in Mount Pleasant.
The detoxification process from opioids is not a pleasant one, but it is usually not medically dangerous.
“There are common symptoms that can occur during opioid detox from opioid withdrawal. Severity depends on a few things like length of use, concentration, dose and other underlying medical concerns. The common signs and symptoms include increase in heart rate, blood pressure and body temperature, gastrointestinal symptoms like diarrhea, runny nose, anxiety and watery eyes, to name a few. The main concern during opioid detox is to improve comfort and severity of symptoms,” said Lantana Recovery Assistant Medical Director Svetlana Stuck, P.A.
While there can be underlying health issues or circumstances that can make detoxification more challenging for patients and providers, medically supervised detox can also be a more comfortable experience for patients and provide a stronger start to their recovery process.
“There are two main components to consider for medical supervision during opioid detox – safety and comfort. During detox, there is potential for safety concerns depending on the severity of symptoms. When detox is medically supervised, the client can have more access to medications that can be helpful in decreasing the symptoms of detox and improving comfort. A successful detox can also help set a positive foundation for recovery,” Stuck said.
“For that reason, compassion is at the core of everything we do at Lantana Recovery. We meet people who are going through one of the most difficult experiences a person can go through. We want them to know that they are not alone,” Rosa added.
Tolerance levels are also an issue for chronic opioid users, which leads patients to take more opioids for relief even when they already know they may have an issue. Opiates often are prescribed to treat chronic pain. However, extended use can lead to greater tolerance, which decreases the medication’s efficiency in treating the pain – so patients require more medicine to obtain relief. Eventually, it could become unhealthy and unsustainable for patients to continue to use opioid medications as treatment for pain, because they can become physiologically dependent on them.
“We’re seeing they’ve built up a tolerance for whichever substance they use,” explained Adult Services Director Jessica Owens of the Phoenix Center in Greenville. “We also see withdrawal symptoms, and it makes people feel awful. There’s also the rebound effect of pain.”
To provide options for patients, the Phoenix Center offers a variety of substance use disorder treatment programs, including a five-day program that immediately lowers the patient’s tolerance of the opioid medication. There also are outpatient services with the Medication Assisted Treatment program, which provides medications such as suboxone or buprenorphine to help patients taper off gradually and avoid a sudden rebound of severe pain.
“The outpatient with MAT is the gold standard. It helps with cravings and withdrawal symptoms and allows patients to get into treatment and focus on treatment because they’re feeling better,” said Owens.
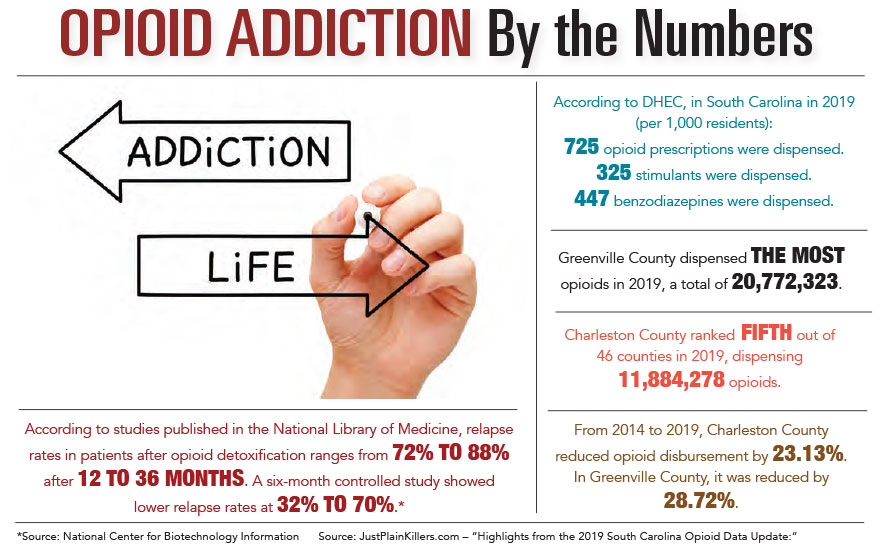
Providers say that the ability to focus on continued treatment during and after detox is crucial to a patient’s recovery, and the data supports it. According to a study published by the National Institutes of Health, relapse rates after opiate detoxification range from 72% to 88% after 12 to 36 months. A six-month study showed lower relapse rates at 32% to 70%. This highlights the importance of continued care long after the detox process is complete.
“Due to the rate of return to use of opioids after detox, MAT is considered a best practice for someone with an opioid use disorder to utilize in conjunction with counseling and treatment services. Some forms of MAT used to assist those with opioid use disorders include suboxone, methodone, vivitrol and naltrexone,” added Michael McLain, director of local provider relations for the Phoenix Center.
“Detox is only the beginning of recovery, and many of the issues which contribute to relapse persist well into early recovery. Following detox, many find professional counseling and support groups vitally important as they navigate the ups and downs of early recovery,” said Bob Hennen, LPC, LAC, and executive director of Lantana Recovery.
“Continued counseling can help address co-occurring conditions such as depression and anxiety. Counseling can help the family learn how to support someone in early recovery, as well as work through the stress and strain substance use places on a family system. Professional support can help build positive coping skills such as stress management strategies and other relapse prevention skills,” he added.
If opioid medications have a high risk for developing addiction and substance use disorders, then why are doctors still prescribing them, especially for long-term conditions such as chronic pain? Todd Joye, M.D., owner of interveneMD in Charleston, has been treating patients with chronic pain for 20 years, most of them with spine conditions.
“There’s not an easy answer to this complicated and polarizing issue. Opioids are still instrumental in the management of acute and cancer pain, as well as some chronic pain conditions, so they shouldn’t be abandoned completely, nor should we treat all those who do take them as abusers. But we can be more aware of the risks of taking them and try to monitor patients better than we did 20 years ago,” said Dr. Joye.
There is also an emphasis on providing other treatments in addition to, or instead of, prescribing opioids as the first option for pain relief.
“I tell patients that we’re giving them a tool belt, and the more tools – treatments – we can get on it, the better job we can do taking care of their pain. Now more than ever, opioids only take up a small portion of that tool belt, and we’re making sure that if we have to use opioids, we’re using the smallest dose possible and that we’re investigating, offering and employing other avenues for relief.”
For more information on the opioid detoxification and recovery process, contact the Phoenix Center in Greenville at 864-467-3790 or visit phoenixcenter.org. In Mount Pleasant, contact Lantana Recovery Center at 843-352-9982 or visit lantanarecovery.com.
By Katie Thompson
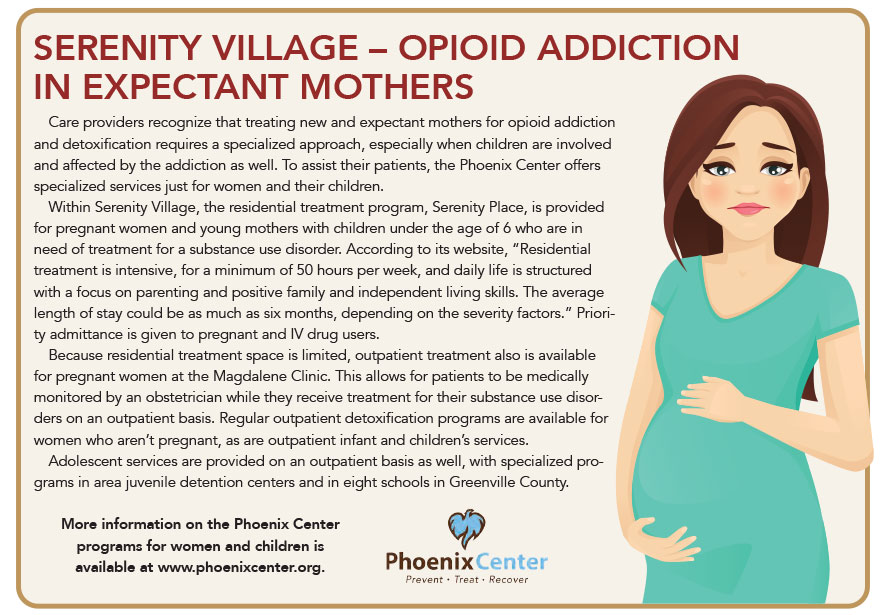
More information on the Phoenix Center programs for women and children is available at phoenixcenter.org.