Do you snore when you sleep? Does your bed partner? You’re not alone. Almost from time immemorial, nocturnal noise-making has been so common that it has created such familiar expressions as “sawing some wood” and even the euphemism for sleeping, “catching some ‘Zzzs’.”
Snoring is a frequent subject of humor. But, in reality, it’s not a laughing matter. Sleep-disordered breathing can have a host of health and even life-threatening side effects, among them morning headaches, dry mouth, overall fatigue and even drowsiness that can lead to such negative outcomes as industrial accidents and automobile crashes.
Worse yet, snoring can be a marker for the condition obstructive sleep apnea, which can be a factor in diabetes and heart disease and can lead to death.
The good news is that not all snorers will develop OSA. On the other hand, most OSA sufferers also snore.
Snoring is a symptom that indicates your airway is closing off or diminishing. There are a number of possible causes for this, ranging from the size and shape of your tongue and tonsils to fat accumulating in the area of your windpipe.
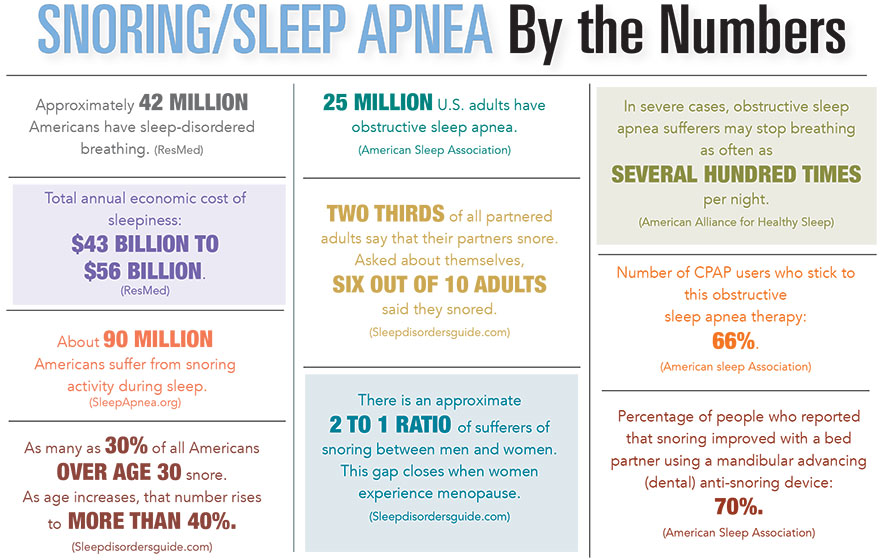
For most patients diagnosed with OSA, the conventional treatment has been the CPAP (continuous positive airway pressure) device, a full or partial face mask worn during sleep that forces a stream or pressurized air into the airway, helping to keep it open.
Many patients acknowledge the benefits of CPAP therapy but for various reasons cannot wear the mask consistently. For these OSA sufferers, relief may be as close as their properly certified dentist.
Dr. William Healy, a specialist in pulmonary critical care and sleep medicine practicing at the Prisma Health Lung Center at Hillcrest Memorial Hospital in Simpsonville, agreed that dental appliances can be a good treatment option for the right patients.
Particularly for patients diagnosed with mild to moderate sleep apnea, “a dental appliance fitted by a skilled dentist with plenty of experience can also be very effective.”
One of these qualified dentists is Dr. Dana Blalock, a diplomate of the American Sleep and Breathing Academy whose Sleep Better SC practice is on Daniel Island.
While acknowledging that CPAP therapy remains “the gold standard” for OSA treatment, Dr. Blalock stated that “oral appliances can very effectively treat patients with mild to moderate sleep apnea and are a wonderful alternative for those who cannot tolerate the mask.”
That said, Dr. Healy always starts his sleep apnea patients with the CPAP as it is “still the most effective treatment with decades of data documenting effectiveness in ameliorating daytime sleepiness and improving blood pressure along with potential reduction in heart attack and stroke in certain patients.”
To determine whether a patient suffers from sleep apnea and whether that condition is mild, moderate or severe, Dr. Healy relies on a one-night in-lab sleep session or a similar “at-home” session.
Both testing methods, he believes, can be effective diagnostic tools, although the in-laboratory sessions gather more data by monitoring such factors as brain-wave activity and leg movements during sleep.
If dental intervention is recommended, the patient is fitted with one of several styles of appliance, all of which are similar to the mouthpieces worn by many athletes in sports such as football and boxing. Each is custom-fitted, fabricated to each individual patient, worn only at night and discreet and convenient to use.
Dental sleep medicine experts such as Dr. Blalock always work hand-in-hand with sleep medicine physicians. Dr. Blalock frequently accepts referrals from these doctors and also refers her dental patients to the same specialists when she detects oral anomalies that might contribute to OSA.
She said that she estimates 15% to 20% of the patients she sees on a regular basis are potential OSA patients.
She added that OSA is serious business. Dr. Blalock noted that untreated, OSA “can kill.” The condition and the reduction in oxygen intake it causes make the heart work harder, which can lead to heart failure or stroke. It can also cause elevated blood pressure and has been linked to the development of Alzheimer’s disease.
Dr. Healy clearly does not disparage any technical advances in treating OSA. However, he notes a general inclination among both medical professionals and the general public to always be looking for that silver bullet for improving sleep.
“We often focus on the most complicated solutions to medical problems when there may be simple, albeit less glamorous, techniques that can work very well,” he said.
Among his simple tips for a better night’s sleep are keeping all electronics out of the bedroom, dimming all lights, following a set bedtime routine and working to reduce stress in your daily life.
Dr. Healy further noted that physical activity and weight loss are frequently positive factors in reducing or even eliminating OSA.
“I feel that one of the hallmarks of a good sleep medicine doctor is that he or she discusses with each patient the importance of diet and exercise in dealing with their OSA and explains that in certain cases sleep apnea responds positively to simply adjusting one’s sleeping position from the back to the side,” he said.
Until fairly recently, the doctor observed, “people didn’t think of sleep medicine as a distinct specialty. Some patients even today are surprised to learn that it exists.”
So why did he choose to focus on diagnosing and treating OSA?
“Because it is really rewarding to help people feel better during their waking hours. Treating OSA brings great benefits in terms of energy and quality of life.”
And how about all those TV and radio commercials touting certain mattresses and pillows as critically important to a good night’s sleep?
You might as well stick with what you’re used to because Dr. Healy stated “we just don’t have the data to show that any of those claims are true.”
And the next time you’re having your teeth cleaned, mention any sleep issues to your dentist.
By Bill Farley