Trust your gut. We’ve all heard this advice, but it turns out that “gut feeling” is even more important than you may have thought.
While it’s no surprise that gut health plays a crucial role in digestion, that is far from its only purpose. A healthy gut supports the body’s immune system, improves mental health and helps combat obesity and an array of diseases.
“Our gut health reflects the entirety of our lifestyle,” said Dr. Will Bulsiewicz, a gastroenterologist with Lowcountry Gastroenterology and author of “Fiber Fueled: The Plant-Based Gut Health Program for Losing Weight, Restoring Your Health, and Optimizing Your Microbiome.”
That means people can shape the health of their gut microbiome through diet and lifestyle.
“A healthy gut is central to human health,” Dr. Bulsiewicz said, pointing out that the gut is home to trillions of bacteria, both good and bad, that help digest and extract nutrients from food.
“It’s a symbiotic relationship. Nobody has a problem until it gets misaligned,” added Dr. Stephen Yarborough, a gastroenterologist with Gastroenterology Associates of Greenville.
According to Dr. Bulsiewicz, diet is the top determiner of gut health, and the key is to eat a diversity of plants. He said if we think of food on balance scale, with foods that promote health on one side and those that take away from health on the other, 90% of what Americans consume would fall on the wrong side.
“It’s weighing the scale down heavily in favor of disease,” he said.
Processed food makes up 60% of the American diet. Much of the rest is from animal products, which Dr. Bulsiewicz said studies have shown don’t nurture a healthy gut microbiome.
“You can be healthy and enjoy those foods, but you can’t be healthy and enjoy those foods the way we’re doing it right now,” he said.
On the other end of the scale are the plants – fruits, vegetables, whole grains, seeds, nuts and legumes – which comprise 10% of the American diet. French fries account for much of that 10%, Dr. Bulsiewicz said. He added there’s a special connection between the fiber in plants and our gut microbes. Each plant’s fiber appeals to specific families of bacteria.
“These bacteria are picky eaters. They’re like us. We have food that we like and that we don’t like. Bacteria are like us. They don’t all eat the same thing,” he said. “We need as much diversity within our diet to feed as many unique populations of bacteria as possible. When we do that, we build a diverse microbiome. A diverse microbiome is hearty and resilient and ready for whatever we throw at it.”
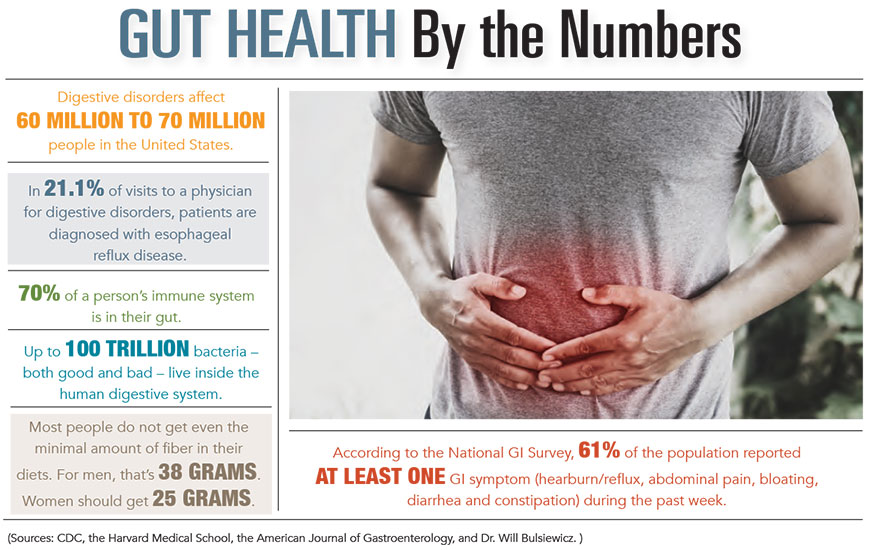
Dr. Bulsiewicz said 97% of Americans are not getting the minimum daily amount of fiber they need – 25 grams for women and 38 grams for men.
“When we’re not getting fiber, we’re not feeding our gut. We’re loading up on processed foods and animal products that have no fiber, and we’re creating a formula for illness,” he said.
Digestive disorders affect between 60 million and 70 million people in the United States, according to the Centers for Disease Control and Prevention. The most common are gastroesophageal reflux disease, which causes stomach acid or contents to back up into the esophagus, and irritable bowel syndrome, a group of symptoms that include constipation, diarrhea, bloating and stomach pain.
The American College of Gastroenterology said IBS is the most common disease diagnosed by gastroenterologists. It estimates that 10% to 15% of adults suffer from its symptoms.
“It’s more of a functional problem than a life-threatening problem,” according to Dr. Yarborough.
But if symptoms persist more than a couple of weeks or are severe, it may be a sign there’s an underlying problem that needs attention, said Dr. Lori Robbins, a gastroenterologist with Charleston-based Palmetto Digestive Health Specialists. Symptoms that should prompt immediate medical care include weight loss without a good reason, blood in the stool, black stool, severe vomiting, severe stomachaches and trouble swallowing food, Dr. Robbins said.
“Both IBS and inflammatory bowel disease interrupt a person’s daily lifestyle,” she said. “With IBS, there are not typically long-term physical consequences if left untreated. Inflammatory bowel disease is an inflammatory disorder that can have potential long-term complications. There is no cure, but there are medicines to treat it.”
Besides eating more fiber and cutting back on processed foods, you can improve your gut health by avoiding unnecessary antibiotics, which kill good bacteria as well as bad, Dr. Yarborough said. Getting enough sleep and staying hydrated also promote gut health, he added.
Stress affects gut health, and Dr. Bulsiewicz said he’s seeing more patients with gastrointestinal problems having flare-ups during the coronavirus pandemic.
“We’re all feeling the threat of COVID-19, whether it’s from a health perspective, financial stress or change in routine. Stress can alter the balance of microbes and induce dysbiosis,” he said.
In times of stress, we often reach for junk food and alcohol, something that Dr. Bulsiewicz said is no coincidence because our microbiome controls our cravings.
“Now more than ever requires a conscious effort to nurture a healthy gut microbiome,” he concluded.
By Cindy Landrum