Clinician burnout impacts providers and patients but also the health care system, and the additional strain on clinicians during the COVID-19 pandemic are unparalleled. Fortunately, health care leaders are looking after the well-being of clinicians in South Carolina with the Thriving Workforce initiative provided by the South Carolina Hospital Association’s Working Well division.
“The Thriving Workforce initiative is coming out of Working Well and the SCHA with our valued partners. Working Well is SCHA’s initiative to help organizations build cultures that support the well-being of their employees. It’s different than a direct-to-employee wellness program; it’s really to help the organization set up the workplace environment, cultures and attitudes that help employees thrive at work,” explained Working Well Director Jen Wright.
The Thriving Workforce initiative was created to focus specifically on the well-being of South Carolina’s hospital workers, and the work group includes health care leaders from across the state. The initiative was launched in 2019, shortly before the arrival of the global pandemic, and couldn’t have come at a better time, especially for the nurses and support staff that make up the majority of health care workers.
“We are really making a conscious effort with the Thriving Workforce initiative to incorporate all clinicians because everyone is a valuable member of the care team. Each person and each organization has a role to play,” Wright added.
Rachel Brown, M.D., medical director of prevention and wellness at Prisma Health and a Thriving Workforce work group member, explained that what causes burnout can make an impact across organizations: “Those drivers are the same for all of us, whether we’re physicians, nurses or therapists or even our administrative staff or our front desk folks.”
In her work providing health and well-being programming and strategy to more than 17,000 employees, Susan Johnson, Ph.D., director of health promotion and assistant professor of graduate studies at the College of Health Professions at the Medical University of South Carolina, shared that decompression and autonomy are two causes of burnout.
“Decompression is, ‘When I leave work, I can leave it behind.’ That’s what a lot of our clinicians, in particular physicians, struggle with,” Dr. Johnson explained.
The well-being and needs of health care workers have been especially stressed by the mounting pressures of the COVID-19 pandemic. According to Wright, organizations that create a culture of trust and communication, especially in uncertain times, also can create a stronger workforce.
“Some of the things we’re hearing are the need for multidirectional communication, just in general and in uncertain times. When people are unsure of what’s going on, even if you don’t have the right thing to say or what you feel like might be the perfect thing to say, keeping those lines of communication open, helping people feel included, informed and trusting of what the leadership is doing,” explained Wright. “The more resilient populations are housed in organizations where the trust and feeling of valued work is already there.”
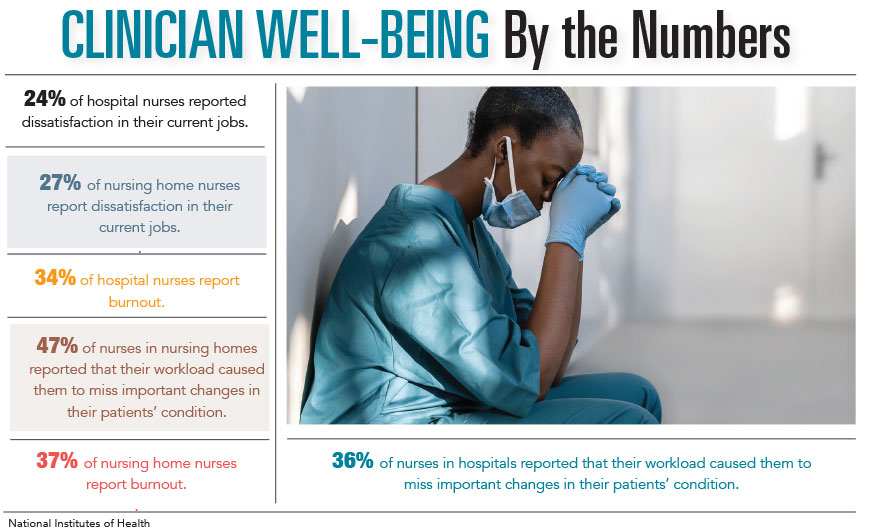
The approach of the Thriving Workforce initiative is based on extensive research on the well-being of health care professionals, which includes the Stanford WellMD Professional Fulfillment Model created by Stanford Medicine, as well as strategies from research provided by the National Institutes of Health, among others.
The Stanford Model emphasizes a three-part approach to generating professional fulfillment in health care professionals. Creating a culture of wellness, the efficiency of practice in workplace systems and personal resilience skills of individuals are the three areas with identifiable key success factors that lead toward professional fulfillment.
Creating systemic changes and generating leadership support are vital to organizational health, but it also impacts the resilience of individual employees. Cultures that support their employees by providing financial and emotional counseling and even basic self-care assessments enhancing their employees’ well-being.
While large-scale changes to organizations can have a direct effect on employees, Dr. Brown emphasized that there still needs to be individual work unit interventions to address the unique needs of the unit and its specialty.
“We could create wellness plans for 30,000 team members, but it’s inefficient and it puts the onus on them, as if their well-being is their full responsibility and not their environment,” she said, “Often, systems interventions are too general, and they aren’t as tailored. There’s no one right answer, even within an organization.”
Creating tools for organizations to support the well-being of their employees isn’t a one-size-fits-all approach, and the strategies the Thriving Workforce initiative brings to hospitals will reflect that.
“If we’re supporting a work unit, we are going to tailor a plan that is best for them. There will be tools that can help with that in the Thriving Workforce toolkit,” Dr. Brown added.
By Katie Thompson