As if avoiding or surviving COVID-19 has not been challenging enough, the collateral effects of the virus also have been noteworthy. Perhaps you remember how, in early 2020, hospitals, clinics and doctors’ offices suddenly became frontline MASH units – places that otherwise healthy people should avoid at all costs. It seemed as if overnight our trusted health care system had switched from taking care of everyone to strategically focusing on the unexpected influx of seriously ill COVID patients. Whole sections of hospitals were converted; families and loved ones were banned; and non-life-threatening surgeries and medical procedures were temporarily postponed. It was a frightening time.
However, as the year painfully dragged itself forward and better treatments emerged for COVID, health care returned to some level of normalcy. Surgeries were rescheduled and standard medical procedures were available once more. But where were the patients?
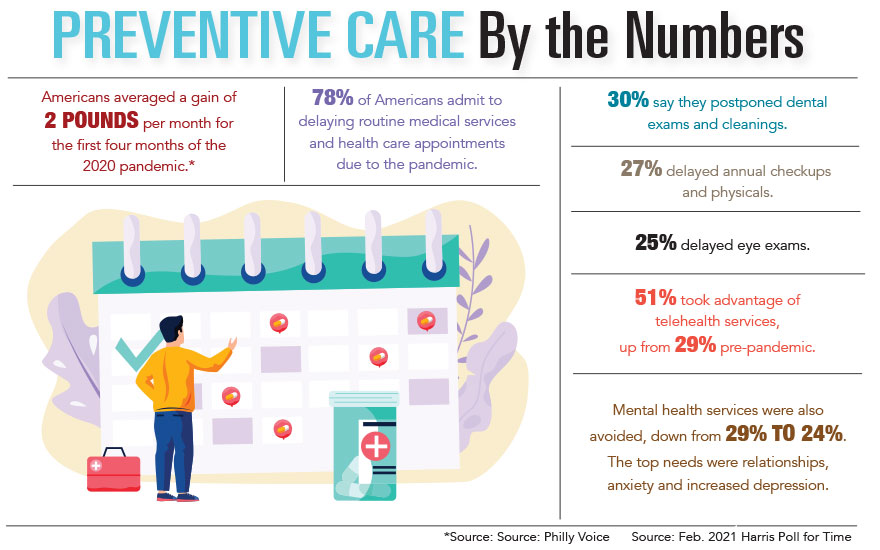
According to a recent Time-Harris Poll, a staggering 78% of American adults decided to delay routine medical services and health care appointments due to the COVID-19 pandemic. They avoided dental checkups and cleanings mostly, followed by annual physicals and eye exams. They also dodged mammograms, colonoscopies, diabetes care, other routine screenings and mental health appointments.
Radiologist Brian Mahon, M.D., of Trident Breast Care Center, has seen the same hesitancy to come in for appointments, especially among the older, high-risk demographic. Worse, he said, “We only know the ones who put off coming in but did eventually come. We have no way to account for those who were planning to schedule a mammogram and just decided not to call us. In this area of proactive health care, six months is a significant time. Catching potentially cancerous changes early and quickly is extremely important.”
While there is some controversy in the medical field about just how often a woman should have a mammogram, Dr. Mahon recommended yearly visits after age 40 and more often if a woman falls into a higher-risk category. He has been pleased to see a gradual return to scheduling checkups and routine screenings.
Cesar Santiago, M.D., a colorectal surgery specialist at Trident Medical Center, is also experiencing a gradual return of patients after months of fewer visits. Initially, the number of elective surgeries dropped significantly because patients were afraid to go to medical facilities. Even those dealing with cancer diagnoses were reluctant to seek out continuing medical care.
According to Dr. Santiago, “Because most little polyps can take five to 10 years to become a benign cancer, many patients feel they are safe. However, for the patient who already has cancer or cancer symptoms, a small growth can metastasize in a matter of months, and delayed or postponed treatment can be very serious. This reality becomes even more consequential for seniors over 60, who fall in a higher-risk category but are still hesitant to come in.”
While general use of telehealth has risen during COVID, both Dr. Mahon and Dr. Santiago have found it less helpful in dealing with patients who require physical procedures and monitoring.
Catherine Reinhart, R.N., Trident’s certified diabetes care and education specialist, shared a similar story of canceled appointments, especially during the initial phases of the COVID outbreak.
“I have seen that people were delaying routine follow-up visits as well as elective procedures due to the fear of exposure,” she reported. “However, as time has passed and precautions have been implemented, we are seeing more patients.”
“Furthermore, the Centers for Medicare and Medicaid Services has given a waiver to recognized diabetes education and support programs to provide telehealth to eligible participants. We offer this option to those who are not comfortable coming to the office, who live far from our facility or who may be infected with COVID and unable to come in,” Reinhart said.
While it is impossible to predict the future of COVID-19, Dr. Mahon, Dr. Santiago and Reinhart are optimistic that vaccinations, precautionary safety procedures and other measures will continue to address patient concerns. They encourage those who have been hesitant to reconnect and come back in. Where health is concerned, sooner is always better than later.
By Janet E. Perrigo