With more than 40% of adults in the United States classified as being obese and many more carrying excess weight and dealing with related health conditions, it’s no secret that Americans have been suffering with this escalating epidemic for quite some time.
For those with severe obesity, the most effective, long-term treatment approaches are surgical procedures known as bariatric – or weight-loss – surgery.
John Scott, M.D., a bariatric surgeon at Prisma Health Greenville’s Weight Management Institute, defined the procedure as “surgical treatment for morbid obesity and its associated medical conditions,” including diabetes, high cholesterol and sleep apnea. Bariatric professionals often refer to it as “metabolic surgery” because the procedure changes the body’s metabolism to process food and nutrients differently.
Surgical weight loss treatments are often thought to focus entirely on weight loss, but medical research has discovered additional health benefits derived from modifying the way your body processes food with metabolic impact in addition to a lower body weight.
Prisma Health performs the Roux-en-Y gastric bypass, which involves making the stomach smaller and rearranging the intestine to process food differently. It also performs vertical sleeve gastrectomy, which removes 70% to 80% of the stomach, leaving a slender, sleeve-shaped stomach, that causes a person to feel fuller faster and for a longer time. Both procedures produce favorable changes in appetite hormones, so a person feels less hungry and experiences increased metabolism.
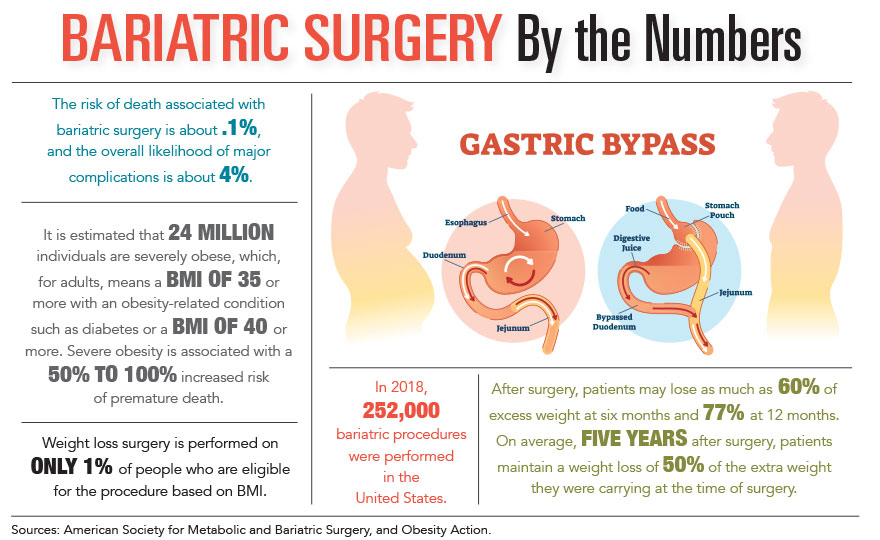
Candidates for surgical procedures include individuals with a body mass index above 40 kg/m2 or those with a BMI between 35 and 40 kg/m2 who have health conditions related to excess weight, such as Type 2 diabetes, high blood pressure or high cholesterol.
“It gives these patients the best chance to put their disease into remission,” Dr. Scott stated.
Nina Crowley, Ph.D., the metabolic and bariatric surgery program coordinator at the Medical University of South Carolina, is part of an interdisciplinary team of surgeons, nurses, behavioral psychologists, nurse practitioners, registered dietitians and patient navigators who work together to educate and support patients as they embark on a journey to improve their health and well-being for the long-term.
MUSC’s program also performs bypass and sleeve surgeries and is one of the few centers in the Southeast offering the duodenal switch procedure, a complex weight loss surgical procedure geared toward patients with more weight to lose – a BMI over 50 kg/m2 – and Type 2 diabetes. After performing a sleeve gastrectomy, surgeons bypass part of the small intestine, resulting in a shorter pathway where food gets digested and less absorption of nutrients. All patients work with their dietitians to take appropriate vitamin and mineral supplementation for life after surgery.
MUSC utilizes innovative robotic surgery technology for the duodenal switch, which provides more precision, flexibility and control. Rana Pullatt, M.D., MUSC’s director of robotic and bariatric surgery, was the first doctor to perform the surgery in South Carolina in 2015 and is internationally recognized as an expert in robotic surgery for both primary and revisional bariatric procedures.
While having health conditions related to excess weight is generally required to have the surgery, Dr. Crowley noted that “earlier intervention generally results in better outcomes” and shared that the adolescents who have had weight-loss surgery reap tremendous health and quality-of-life benefits. Developed for patients beginning at age 13 who meet the requirements, the comprehensive adolescent program relies on telehealth visits, additional check-ins and more interaction with dietitians.
Dr. Scott described bariatric surgery as “incredibly safe,” which he attributed in part to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program, which accredits bariatric surgeries countrywide and enforces national standards and quality control to help ensure patients receive safe and quality care.
“The 30-day mortality risk is less for bariatric procedures than it is for gallbladder removal and knee replacement,” noted Dr. Crowley.
Most patients are up and walking the evening of the procedure and go home the day after, though many people take a week or two off from work following surgery to recuperate fully, said Dr. Scott. After having bariatric surgery at MUSC, patients remain connected with their medical, nutritional and behavioral health team for the long-term.
“Obesity is a chronic disease,” remarked Dr. Crowley. “These are our patients for life.”
Dr. Scott characterized gastric bypass surgery as a “game changer for the treatment of diabetes,” with 60% to 80% of patients seeing their condition disappear within weeks of surgery. MUSC views surgery as the catalyst to facilitate change, and maintenance is a long-term commitment. While the surgery allows a person to feel fuller on smaller amounts of food for longer, optimizing the nutritional value of those few bites and other positive health behavior changes take planning and prioritizing. Behavioral psychologists continue to work with patients in shared medical visits after surgery to help them adapt to new lifestyle changes.
Greenville’s Bee Healthy Clinics, whose medical director is a bariatric physician and member of the Obesity Medicine Association, sees bariatric patients in both pre- and post-surgery stages.
Amanda Groome is a nurse practitioner with Bee Healthy, which serves people of all ages and health levels who need accountability or support with weight loss and weight maintenance issues.
Individuals visiting the clinic pre-procedure generally seek to incorporate healthy habits before undergoing the procedure. Others gain some weight back after surgery, and Bee Healthy helps them change their sedentary behavior, said Groome. This entails getting patients moving, starting them slowly with 15 minutes of walking, four to five times a week.
“Setting realistic goals and expectations and meeting them is important,” stated Groome.
Like MUSC, the clinic regards psychology as a major weight loss component, so it also addresses depressive symptoms that may occur after bariatric surgery. Additional key factors post-surgery include managing food choices and ensuring people are taking the vitamins and supplements that bariatric surgeons recommend to avoid risk of B12 or iron deficiencies.
The clinic helps people make gradual, healthy lifestyle changes that they can follow long-term, such as portion sizing and reducing simple sugars.
“Small changes make a difference,” said Groome.
While metabolic and bariatric procedures offer numerous benefits, insurance coverage presents a major obstacle for many who might be able to benefit. Working together, Drs. Scott and Crowley are passionate advocates for reducing insurance barriers and increasing access to appropriate obesity care in South Carolina.
Additional Sources: MUSC, Penn Medicine and Obesity Action.
By Colin McCandless